Paramedic
A paramedic provides advance levels of care in times of medical emergencies and traumatic situations.

THE RISKS AND REALITIES OF FALLS IN THE ELDERLY AND HOW ALLIED HEALTH PROFESSIONALS SUPPORT PREVENTION

The number of people in the UK population, over the age of 65 continues to increase. Currently 19% of the population is over the age of 65, but in the next ten years this will have increased to 22% (1). As a part of the normal ageing process, people’s physical functions, such as strength, swiftness and stamina, are likely to decline slowly. This can strongly influence coordination, balance, confidence and physical abilities resulting in an increased risk of falls.
Elderly people also have a natural decline in appetite due to physiological changes in the digestive system, hormones, and senses such as smell and taste, which increase the risk of malnutrition (2). Malnutrition is rising issue in older people and has a direct impact on the body’s composition, such as loss of muscle mass. This loss in strength increases the risk of falls (3). Malnutrition also causes the loss of bone mass and density, also known as osteoporosis. Osteoporosis is when the bones become fragile and more susceptible to breaking, making them more likely to break as a result of a fall (2,4).
Therefore, adequate energy from calories, protein and other nutrients from food are vital in supporting older people to maintain as much muscle and bone strength as possible.

Older people are also at increased risk of dehydration due to reduced sensations of thirst and kidneys work. Kidneys and hormones play essential roles in helping the body regulate fluid balance, but the efficiency of both decline with age (5,6). Dehydration can cause symptoms of dizziness, confusion and fatigue, which increase the risk of falling (4).
At any age, someone may suffer from a fall with various physical and mental consequences. However, as people get older, these consequences are likely to be far more severe. For example, an elderly person is ten times more likely to be hospitalised and eight times more likely to die as a result of a fall than a child (7).
In the UK, 30% of people aged 65 to 80 and 50% of people aged 80 and over experience a fall at least once a year (8). Once someone has had a fall, they are 66% more likely to have another fall within a year (9).

Almost 40-60% of the unintentional falls experienced by older people result in injuries that require medical treatment. Many of these injuries are usually minor, such as cuts, strains and bruises. However, others experience head injuries or suffer from hip, shoulder and wrist fractures that require prolonged hospital stays and long-term rehabilitation (10). In 2003, there were over 600,000 A&E attendances and 200,000 hospital admissions from falls (11).
In addition to physical injuries, an individual may have an increased fear of falling again, which negatively impacts on daily living activities, self-confidence, and quality of life. This also increases their dependence on others.
I am afraid of falling again, especially when I am outside the house and I am alone. When I fall, then you never know, maybe I will fracture my hip (12)
The incidence of falls has been recognised to be influenced by medical, behavioural and environmental factors. Medical-related factors such as muscle weakness, impairment in balance, foot problems, visual problems and use of medications are most commonly associated with falls. However, a person’s behavioural actions, such as a inactive lifestyle, alcohol consumption, smoking or taking excess medication, are also predictable risks. Finally, the environmental factors that increase risk include: living in poor housing conditions with hazards and obstructions in the home, having limited access to health services, or lacking social interaction (13).

The risk of falling increases as the risk factors add up. For example, an individual with no identified factors has an 8% chance of falling but this increases to 78% when four or more risk factors are present (14). This highlights the potential need for increased medical attention within this population and preventative practices to allow for a healthier, happier and safer later life.
I stay at home more often and don’t visit my friends anymore. I am afraid to fall when I go out (12)
In order to minimise the risk factors and help prevent falls within the elderly population, many factors need to be thought about. Prevention should focus on providing the following key areas:
Numerous health professionals are needed to provide the different types of support required to lower risk and help prevent someone from having a dangerous fall. Some of these are allied health professionals and others are a part of the wider multidisciplinary team working in healthcare.
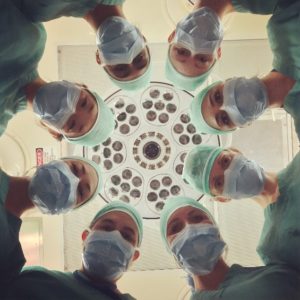
In the unfortunate event that someone does fall, this will require involvement of additional health professionals to support the treatment of injuries, help with recovery, as well as help prevent a future incident.

General Practitioner (GP)
GP is often the first point of contact and is responsible for obtaining routine health screening and assessing the risk of falls among older adults. GPs can review medications and make changes to minimise potential side effects that affect balance and coordination. A GP can also refer people at risk to other healthcare professionals, such as the AHPs discussed above, that specialise in preventive fall practices in the community (16).

Pharmacists
Pharmacists specialise in pharmacology, which is the science of drugs and medication. They can provide information on medications and their possible side effects and interactions.

Social workers
Social workers work with people and aim to improve people’s lives by finding solutions to their problems and supporting them to live independently. In the area of falls, they work particularly closely with occupational therapists to make sure a person’s home is as safe as possible for them to live in.
References: