Vanessa Maynard
Dietitian

Working in Mental Health and Learning Disabilities

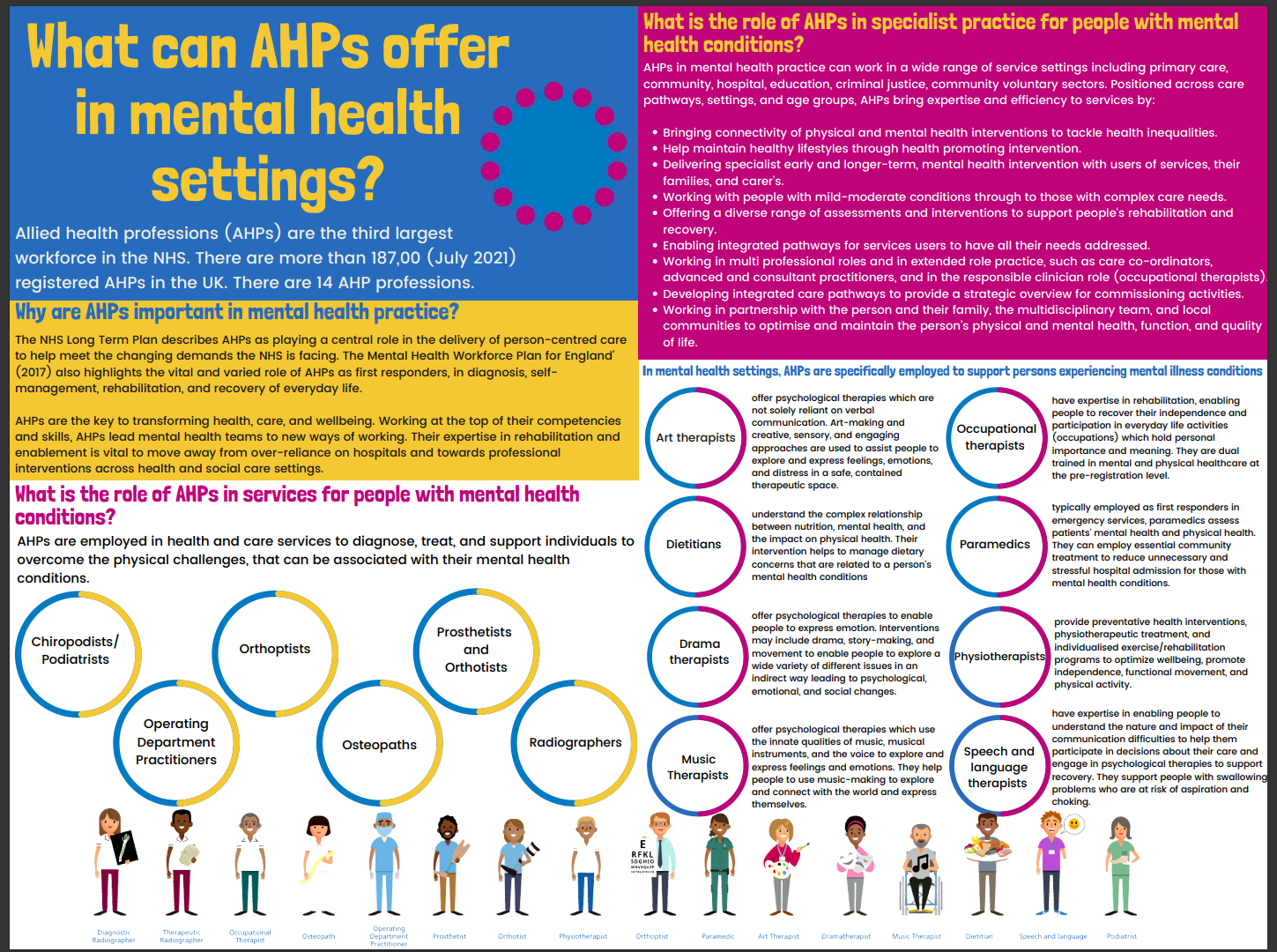
Allies Health Professionals (AHPs) work within a rich variety of settings including acute hospitals, community settings, local authority, charities, schools, prisons, education – just to name a few.
Depending on their profession and the setting they work in, the type of role can differ fairly significantly.
A setting we are going to focus specifically in this article is Mental Health and Learning Disabilities.
The most common Allied Health Professional role in mental health is Occupational Therapy, with approximately half of all qualified Occupational Therapists specialising in this area.
The other AHPs who are more likely to work in mental health are:
Allied Health Professionals use a holistic approach to healthcare and aim to improve individuals’ health and wellbeing, supporting people to live full and active lives. Allied health professionals working in mental health and learning disabilities, use their specialist skills to:
We spoke to Martha Benfield, Student Committee member of the British Dietetic Association Mental Health Specialist Group and asked her a few questions about working as an Allied Health Professional in Mental Health.
Take a look at her perspective of allied health professionals in mental health and learning disabilities and the holistic care they provide to service users:
Service users accessing mental health services are there for that primary reason – to have care and treatment around their current mental health condition(s). They may have voluntarily entered the service, be referred into the service, or have been brought into the service under sectioning by authorities in line with the Mental Health Act 2007. This creates a wide span of service user perspectives, which, alongside the condition a person has, plays a role in how a service user may interact with their care. Some may have care in their own home, some may be in a specialist hospital setting that they can leave at any time or at specific times only, and some may be in hospital without the ability to leave.
Although closely related to mental health services, eating disorder services are usually separate entities, with specialists providing this care in both community and inpatient settings. However, as with physical health settings, service users accessing wider mental health and learning disability services may also present with an eating disorder.
Regarding learning disabilities services, these are specialist services positioned to support individuals meet their care needs. This may mean that service users are referred from general care services into this specialist care, where support can be tailored to individual needs. Again, these services may be provided in the community, in nursing homes and schools for instance, and in inpatient settings, and although also relevant in all health services, here, the Mental Capacity Act 2005, advocacy, and carer relationships are significant to the care process.
Service users accessing mental health services are there for that primary reason – to have care and treatment around their current mental health condition
The big difference is the key focus of care – mental health. This means that the majority of the professionals in the environment are positioned to give care around service users’ mental health condition(s) – for instance Mental Health Nurses and Psychiatrists. As some Allied Health Professional (AHP) training is centred around providing therapy that predominantly harnesses mental health or mental health outcomes, this may feel more like second nature! However, for other AHPs, whilst their training may encompass mental wellbeing or health, the outcomes of therapy are centred in physical health – so this setting may feel very different.
Similarly to some physical health settings, the role of the AHP is complimentary to the main focus of care. So, in mental health services, AHPs may have a stronger focus on physical health compared with other professionals in this setting, with this therapy supporting care plans service users have in place for their mental health treatment. Opposingly to physical health services, this can mean relevant AHPs ‘champion’ physical health within multi-disciplinary teams (MDTs) and with service users in their holistic care.
A further key difference is time. Often in this setting, there may be more flexibility around consultation timeframes when working with service users compared with those that may be present in physical health settings. Due to this, both mental health and learning disabilities services are positioned to encourage creativity and to use varied, specialised communication skills and techniques in order to effectively engage and support service users achieve their goals for care.
Additionally, in certain mental health services, there are increased security protocols when compared with physical health environments, including secure entry to hospitals, locked wards, personal alarms, and relevant staff training.
Mental health and learning disabilities services encourage creativity and focus on using varied, specialised communication skills and techniques in order to engage with their service users and effectively support them achieve their goals for care
There is no doubt that these are challenging settings to work in. Service users may have significant history of trauma, express challenging behaviours, and staff may be exposed to distressing situations. Therefore, as in physical health settings, it is important for the potential impact on staff to be considered.
For instance, individual Trusts may put options in place for staff such as regular practice supervision with psychologists or psychiatrists, options for psychological support, and more frequent opportunities line management contact.
Further to this, as service user care can be complex and involve other external agencies, there may be important MDT links which provide opportunities for collective professional support.
A useful place to start could be looking into professional bodies dedicated to your profession, as there may be a specialist group or association that supports professionals in these areas, and provides information and resources.
Take a look at the videos and additional resource links below, along with the inspirational stories of some of our allied health professional staff working in Mental Health and Learning Disabilities.
Take a look at our inspirational stories from allied health professionals working in Mental Health and Learning Disabilties
The Value of AHPs in Mental Health Recovery - Martha's Story
The Value of AHPs in Mental Health Services
AHP Careers in Mental Health - Physiotherapy
AHP Careers in Mental Health - Occupational Therapy in Perinatal Services
AHP Careers in Mental Health - Dietetics