Maariyah Nazir
Physiotherapist

Physiotherapy Role and Tracheostomy Patients on the ICU
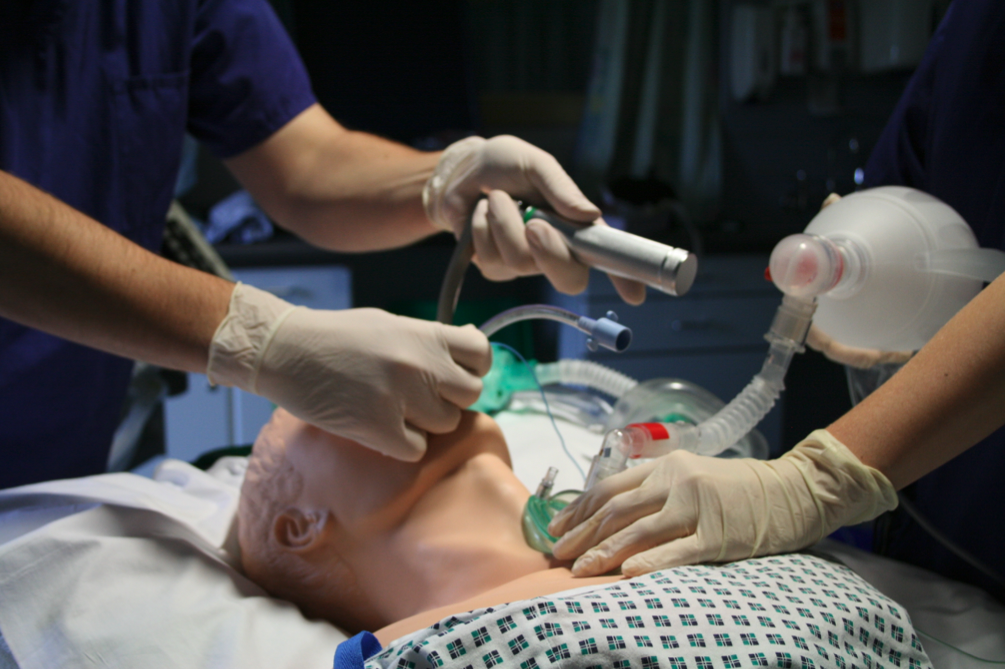
Patients are critically unwell, often with severely reduced consciousness and requiring mechanical ventilation as they are unable to breathe independently. They may have multiple tubes and wires attached to them and multiple screens monitoring their vital signs and respiratory condition. Their medical condition can change very quickly, and they require a huge amount of specialist input to keep their body functioning as it recovers. Physiotherapists contribute to the care of such patients in the following ways:
A tracheostomy is an incision made in the neck of a patient to create an artificial airway. A tube is inserted into the tracheostomy which allows the patient to be mechanically ventilated or to breathe independently. There are several reasons why a tracheostomy might be performed:
Tracheostomies are usually performed while patients are on the ICU but can remain in place once the patient is transferred to ward-level care, and even once they go home. However, the objective in most cases is to wean patients off the tracheostomy as they recover, and their health and strength improves.

A physiotherapy degree course covers three core modules:
Tracheostomy management is part of respiratory physiotherapy but the tracheostomy patient is likely to have neurological or movement issues as well.
Tracheostomy patients may require regular monitoring, ventilator support and close supervision during their hospital stay, or they may be more independent if the tracheostomy is well established. Tracheostomies can be in place for a few days, months or for many years. For all patients, a physiotherapist will help to manage their respiratory function, which many include using airway clearance techniques, weaning from a ventilator and breathing pattern assessments.
When assessing and treating a patient, we can use techniques including manual hyperinflation, active cycle of breathing techniques (ACBT), postural drainage and suctioning. These approaches all aim to prevent the accumulation of mucus in a patient’s lungs to avoid infection or deterioration. Physiotherapists will also be involved in the decision to remove a tracheostomy, which is called decannulation. This involves a multidisciplinary evaluation of how well the patient is managing with their tracheostomy, whether they can clear their own chest secretions effectively, and how much oxygen support they still require.

Working within a multidisciplinary team (MDT) is essential in optimising patient care and maximising outcomes. We work closely with other clinicians including nursing staff, resident doctors and consultants of various disciplines, and a range of other Allied Health Professions.
I had the opportunity to work on the tracheostomy team when I was on my first placement as a physiotherapy student. As this was my first clinical placement, I had no idea what to expect, but I was very interested in respiratory physiotherapy and was excited for the experience.
I found being a student in this environment was so insightful, yet challenging, to be present with critically ill patients, a busy ICU environment, and difficult decisions to be made and conversations to be had. It was so important to be exposed to a physiotherapist role in this scenario, as previously I had no idea this was within our scope, and many other people thought the same.
This experience opened many learning opportunities for me, from physiological knowledge development, emotional intelligence challenges and the ability to develop as both a student and a clinician. Most importantly, this placement exposed me to the MDT and how vital each individual is to the team, to maintain a smooth working environment which prioritises patient care. This niche area has opened my eyes to the wide world of physiotherapy, and has informed my current area of interest, which is low level patients with respiratory difficulties.
I undertook a 6-week placement in the Neurosurgery department as part of the Physiotherapy ‘Trache Team’. I spent mornings on the Neurological Intensive Care Unit treating patients who had varying degrees of brain injury, assessing the state of their respiratory systems, and treating their symptoms accordingly. Within a few days, I was confident in performing multisystem assessments, gathering information from the bedside monitoring equipment, and using deep suction to remove excess sputum from patient lungs.
I got excellent training in managing tracheostomies including how to progress a patient from first insertion through to them being ready for removal, including identifying and treating setbacks. Several of the tracheostomy patients became well enough to step down to ward-level care and I was able to continue managing their tracheostomies as well as being involved in their neurological physical rehabilitation. I was very proud to be able to remove the tracheostomy for one patient who I’d worked with since my first day.
I loved the ICU environment, and it was also a huge honour to meet patients and their families and be part of helping them to recover from life-threatening illness or injury. I had a brilliantly supportive educator who encouraged as much independence as possible in such a technically complex environment. I also worked closely with OTs and SALTs to rehabilitate the patients. By the end of my placement, I felt like I had gained really valuable experience in terms of both clinical and interpersonal skills.
Article written by Olivia Johnson and Kass Evans, Physiotherapy Students.
February 2025
Want to learn more about the role of physiotherapists? Want to find out more about their career path and opportunities available?